Carney Hospital’s emergency department once served 31,000 patients a year. Now, it serves none.
Over the past decade, Massachusetts witnessed the slow and painful death of its largest hospital chain. A few months ago, the Commonwealth finally laid it to rest, leaving a massive vacuum of care in its wake. After years of exploitative financial deals and patient care scandals, for-profit healthcare giant Steward declared bankruptcy in early May, leading to the permanent closure of Carney Hospital in Dorchester and leaving the largest and most diverse neighborhood in Boston without essential care.
The massive building, which once bustled with patients, doctors, and staff, is now empty. On the door, a massive poster read “HOSPITAL CLOSED.” It directs patients to Milton Hospital, another healthcare facility over two miles away. Despite local advocates’ concerns about the closure, the government has remained uninvolved, leaving the region scrambling to find adequate care for its residents.
In healthcare, two miles can mean life or death. A few months ago, Stephen Wood, a nurse practitioner in Dorchester’s Carney Hospital emergency department, saw a patient in critical condition. “[She] never would have made it past our hospital,” he says. “She would have died en route by an ambulance to any other hospital. She had minutes to live.”
The decision to close Carney shocked local residents as well as employees, and will lead to an exodus of healthcare workers from Dorchester, Wood explains. “The services that our hospital provided, they’re all going away, and they’re going to different communities.”
“We were literally just pulled into a room,” Wood says. “Not by any administrators, not by anyone from Steward in an executive position. We were told by a colleague.” By announcing their August 31 closure on July 31, Steward broke the Massachusetts law requiring 120 days notice when essential health services are terminated. Many of the workers decided to take action. “I scheduled a protest as soon as I heard that.”
At the protest, dozens of healthcare workers and local community members alike came out to show how important Carney Hospital was for them. “These are the people who haven’t given up,” Wood says. “They’re taking time out of their busy lives to come out and just show people that, you know, we’re not going down without a fight, and we deserve better than this.”
In mid-August, Governor Maura Healey announced that Massachusetts would seize St. Elizabeth’s Medical Center—another Steward Hospital—and protesters demanded that the state do the same with Carney. “In [seizing St. Elizabeth’s], we are protecting access to care in those communities and preserving jobs, jobs of thousands of hard-working women and men who work at these hospitals,” Healey said.
But this protection was not applied uniformly across the state. Around 1,200 employees will lose their jobs due to the Steward bankruptcy crisis. Resident doctors have been transferred to neighboring hospitals that lack the teaching infrastructure to further their education. Nurses and other healthcare workers are still fighting to receive full severance pay for all former workers of Carney.
More than 150,000 people live in the Dorchester and Mattapan areas, and their access to care will be limited by the hospital’s closure. Though Carney was determined to be “an essential service” by the Massachusetts Department of Public Health, Healey has not put it under eminent domain. Unlike St. Elizabeth’s, no buyers stepped up for Carney, and the state didn’t want to indefinitely manage the hospital. “The state cannot run a hospital. Hospital systems have to run hospitals,” Governor Healey said during a press conference.
The Massachusetts Department of Public Health runs four hospitals, including Lemuel Shattuck Hospital, which has 248 beds and “helps economically and socially disadvantaged patients to get high quality, cost-effective care from a staff that respects their dignity,” according to the DPH website. Carney Hospital had around 150 licensed beds at the time of its closure.
While this crisis unfolds, Healey has not visited Carney Hospital, nor the protests. “She had a responsibility here to do something to try to save these safety net hospitals,” Wood says. “There was plenty of opportunity for her to have done something for a decade, and she’s chosen to turn a blind eye.”
Before Steward’s involvement, Carney was a lively community hospital, according to Karl Odom. He worked as a cardiopulmonary technician at Carney for 46 years and lived in Dorchester for even longer. “The doctors grew up around there, the nurses, everyone that worked there, [there were] whole families who worked at Carney Hospital,” Odom says. “I could see when patients came in, they felt that they were coming into a place that was concerned for them.”
Months after the closure, a Facebook group of over 1,500 members titled “Carney People” remains active. Members post photos and relay information about receiving benefits or compensation for the Steward crisis. Mostly, old employees reminisce over their time in the hospital fondly. “I wonder how many of us met our spouses at Carney,” one member wrote. “I can think of a few, lol.” The post has over 40 comments, each person recounting stories of Christmas parties, the Carney float at the Dorchester day parade, and even meeting their husbands in the hallways.
Once Steward rolled in, the culture changed dramatically. “I had patients who would ask, ‘Who is this Mr. Steward?’—they wanted to talk to him personally,” Odom says. The environment “just wasn’t customer-friendly.”
Carney used to hold Alcoholics Anonymous meetings, smoking cessation classes, and other support groups in the building after operating hours. As Steward took hold of the hospital, these community-centered events disappeared. There were fewer community outreach liaisons, and fewer hospital administrators in general, Odom said. “After a while, the people that came in, they would look at the folks that worked there, the people that worked there, and they say, we’ve never seen a sadder group of people.”
In the years that followed Steward’s acquisition of Carney, the hospital was understaffed and ill-equipped. Nurses were overworked and burnt out. Steward began to hire per diem workers—who weren’t familiar with the community—to care for patients. Fewer physicians had to see even more patients. Over time, the standard of care worsened.
Steward soon fell behind on paying bills, and vendors began to repossess vital medical devices. Doctors became responsible for ensuring they had enough supplies—a relatively easy task for Odom, a technician, but much harder for those in the emergency department. “You always were scrounging around for anything,” he says. “People could see it. And once the community saw it, they got a little skittish and they went elsewhere.”
The dissolution of Carney happened slowly. People realized that Steward was in trouble, but they thought Carney would somehow make it out. “People didn’t believe that in healthcare someone would be that callous and let hospitals and sick people just die,” Odom says. “It can’t be a business. Healthcare can’t be a business.”
Bill Walczak has been community organizing in Dorchester since the 1970s. As a young man, he became the chair of a committee turning a recently closed library into a health clinic. This volunteer position eventually turned into his role as the founder and director of the Codman Square Health Center. “I accidentally got pushed into the healthcare system and wound up staying in it for 42 years,” he says. “It doesn’t make sense to people like me, in the public health world, that we would allow a community hospital in a low-income area with poor health outcomes to close.”
In the 1980s, the patient population of Dorchester began to shift from insured government and union workers to African Americans migrating from the South, many of whom were uninsured. Carney hesitated to adapt to the changing patient demographics, which made it very difficult for the hospital to break even, said Walczak.
Dorchester remains the neighborhood with the highest percentage of Medicaid patients in Boston. Even before the hospital system declared bankruptcy, Steward claimed that “low reimbursement rates” from the state insurance were responsible for lower quality of care. In a January statement to WBUR Boston, Steward claimed that “most community hospitals—including Steward hospitals in Massachusetts—are suffering losses that jeopardize their ability to continue to offer services,” due to the state’s inability to raise insurance reimbursement rates.
Popular
“swipe left below to view more authors”Swipe →
In response to declining funds, Carney Hospital’s former owner, Caritas Christi, produced a 2006 report recommending the addition of acute long-term care services, additional oncology programs, and more imaging centers to improve revenue. Eventually, Caritas Christi CEO Ralph De La Torre decided that the hospital system needed an infusion of cash to grow. He partnered with Cerberus Private Equity, with the intention of buying struggling nonprofit hospitals and turning them into for-profit health centers. This new company was called Steward Health Care, and claimed that it would implement the recommendations of the 2006 report. Within a few years, it became clear that nothing would change. “The issues have been similar for a really long time,” Walczak says.
Long before Brian Thompson, the CEO of UnitedHealthcare, was killed walking into an investor meeting in New York City by Luigi Mangioni with bullets that read “delay,” “deny,” and “depose,” Massachusetts struggled to deal with the consequences of privatized healthcare. Cerberus profited immensely from this perpetually struggling hospital system. Shortly after the purchase, the company began implementing a controversial private equity strategy: sale leaseback. Steward sold Carney Hospital’s land to a real estate investment trust, then leased it back to the hospital. This put Carney under a triple net lease, meaning that instead of owning the land, Carney was now responsible for paying rent, property taxes, and maintenance costs.
Sale leasebacks saddle many hospitals with more costs than they can handle, Mary Bugbee of the Private Equity Stakeholder Project said, especially for safety net hospitals with low margins. The extra costs cut into funds that could go to patient care, more competitive wages, and other capital improvements. “It’s fundamentally extractive,” she said.
The real estate investment trust ended up buying the land of all Steward hospitals for $1.2 billion. Almost half of the proceeds of the transaction, $484 million, went to paying Cerberus investor dividends. All the while, hospitals were struggling to balance rising costs and patient care.
During the onset of the pandemic, Cerberus exited its investment. In the decade that Cerberus owned Steward, its investors made $800 million. Moreover, the company paid $111 million to Steward’s ownership. “Our system is completely and utterly broken,” Bugbee says. “It all comes down to profit, and prioritizing profit over patients, and not having enough guardrails from the states.”
In September, Governor Healey announced the creation of a “working group” to research and address healthcare needs in the Dorchester community. The 1199SEIU healthcare workers union successfully negotiated for former employees of Carney Hospital to have their full PTO paid out, but many are still getting far less than what they are owed. Smaller community health centers in Dorchester have yet to receive any meaningful support.
Now that the hospital has officially shut down, it’s unlikely that it can be seized by eminent domain. The community has been grieving, as Karl Odom puts it. “They lost this job—the job really was their family,” he says. “It is going to be a long time before some people forget what happened and recover from it.”
Milton saw an increase in 20 to 40 emergency visits in the two weeks after Carney’s closure, and has recently requested to double its emergency department due to rising demand. Smaller health clinics like the Codman Square Health Center have also reported an increase in patients following Carney’s closure.
“Our local healthcare system does not have the primary care and urgent care capacity to replace the now-lost Carney services,” wrote Walczak in a column for the Dorchester Reporter. He explains that the community is not prepared to handle urgent care without Carney’s emergency department. At the end of the column, he writes: “A rebuilding of community health capacity is now essential to create a healthcare system for this large part of metro Boston. The community’s residents and healthcare experts—not those who turned their backs on our community—should lead this effort.”
In healthcare, these exploitative practices are pervasive. Across the country, 460 hospitals are owned by private equity, with a company called Apollo Global Management owning around half. Apollo-owned hospitals have received complaints of understaffing, lack of resources, and poor quality of care—all complaints that Steward once received. And over the past few months, Apollo bought the real estate of all Steward-owned Massachusetts hospitals.
“The Massachusetts State legislature just missed a huge opportunity to regulate these types of transactions. Their session closed without any sort of, you know, forward looking legislation that would prevent another Steward crisis,” Bugbee says. “Unless our state legislators and federal legislators do something about it, this tactic is going to continue.”
Private equity hospitals are less safe for patients, according to a Harvard Medical School study. After analyzing millions of hospitalizations, researchers found an increase in hospital-acquired infections in private equity owned facilities. Rhode Island, after facing a similar crisis, enacted a law that would allow the state’s attorney general to closely review any substantial transactions involving for-profit hospitals. California’s state legislature proposed a law that would give the state power to block a private equity healthcare transaction entirely, which was vetoed by Governor Gavin Newsom.
Even after the fallout of the Steward bankruptcy crisis, Massachusetts has not enacted any meaningful legislation to protect healthcare workers or patients from private equity healthcare transactions. Steward’s exit has created a vacuum of care in Massachusetts—a gap that may not be filled for many years.
Despite this, Odom remains optimistic that Dorchester, a community of tough people, he says, will survive the closure. “When they like you, you want ’em in front of you, because they’ll go through a brick wall for you. But they fight when they have to.”
More from The Nation

When social structures corrode, as they are doing now, they trigger desperate deeds like Mangione’s, and rightist vigilantes like Penny.
Caleb Brennan
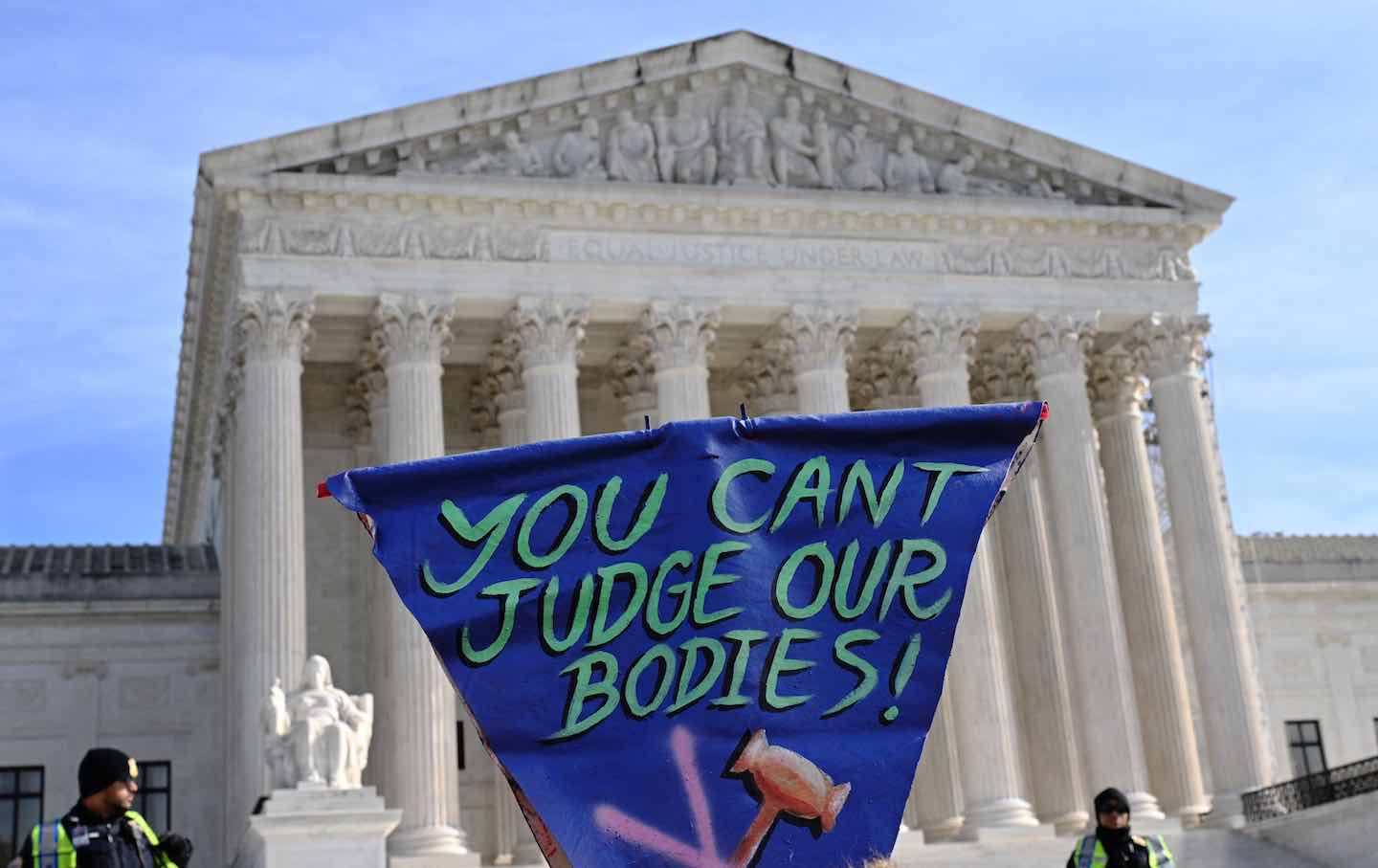
Contrary to what conservative lawmakers argue, the Supreme Court will increase risks by upholding state bans on gender-affirming care.
Aziza Ahmed and Joanna Wuest
Four years after hearing the president promise bold action on student debt, most borrowers are still no better off, and many—especially defrauded debtors—are measurably worse off….
Astra Taylor

There may be a dark shadow hanging over this year’s holiday season, but there are still ways to give to those in need.
Column
/
Katha Pollitt

Thomas and his colleagues at Empowerment Avenue are subverting the established narrative that prisoners are only subjects or sources, never authors of their own experience.
Piper French

While very few Americans would sincerely advocate killing insurance executives, tens of millions have likely joked that they want to. There’s a clear reason why.
Natalie Shure

